Rare ResourcesOur resource page is growing all the time! Feel free to use the search feature if you are looking for something specific. Currently, our resources cover some different types of medical devices and treatments. If you can't find what you're looking for, please feel free to make a suggestion at the bottom of this page, and we will be sure to respond and put it in the works as soon as we can!
|
Searching for Something? |
Feeding Tubes
Many kiddos who battle rare diseases and chronic illnesses require feeding tubes for nutrition. Get more information on feeding tubes here!
-
About the Author
-
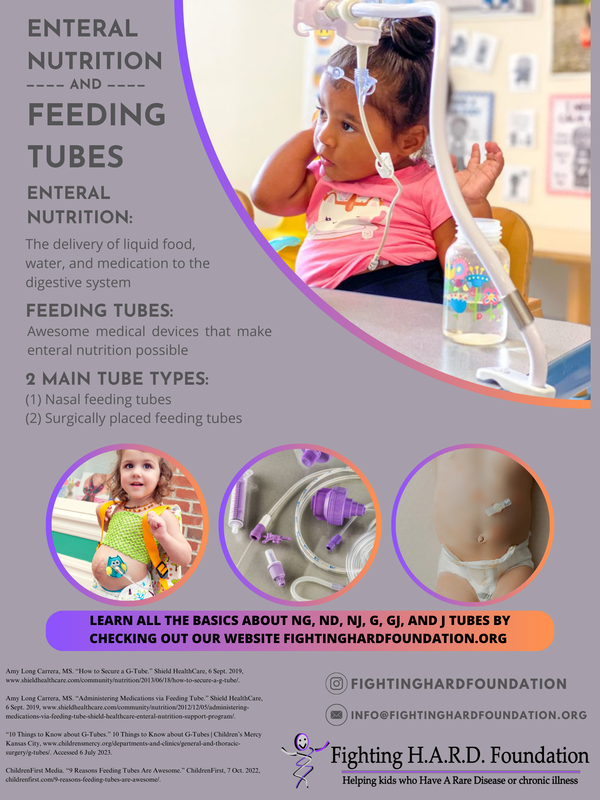
Enteral Nutrition and Feeding Tubes
-
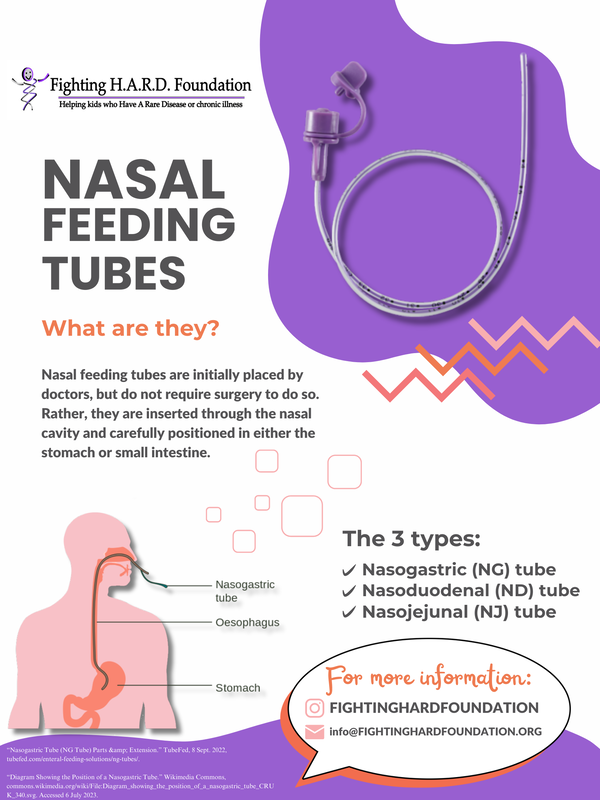
Nasal Feeding Tubes
-
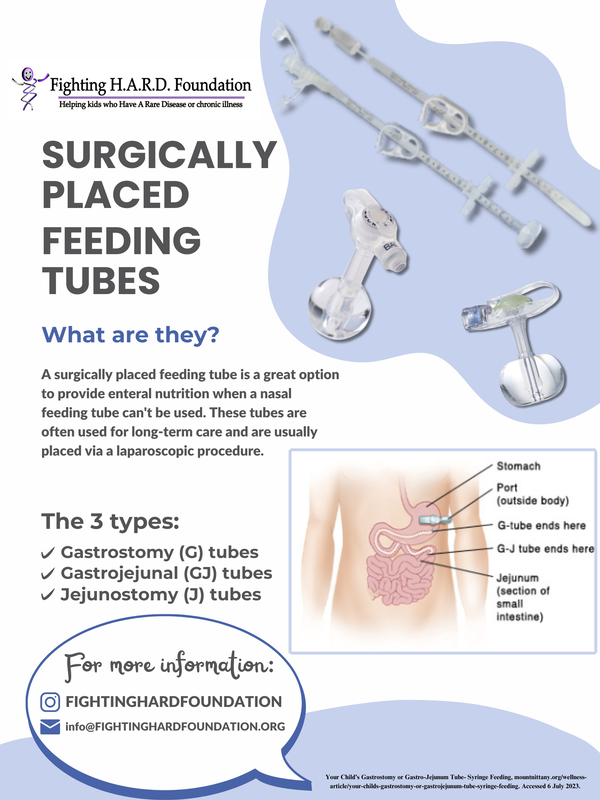
Surgically Placed Feeding Tubes
<
>
About the Author
|
Here, you can find feeding tube resources created by Morgan Burger. Morgan is an undergraduate student at the University of Miami, where she is studying Health Sciences with minors in Biology and Public Health. She successfully completed a summer internship with Fighting H.A.R.D. Foundation. As part of the internship program, she had the opportunity to learn about different medical equipment and devices that many of our rare kiddos need to manage their disease and to create some of the "Rare Resources" for this page! She hopes to work in the medical field after completing her studies. Outside of her education and work, she is the oldest of 3 girls in her family, and she loves to read, go to the beach, and hang out with her friends!
|
|
What is Enteral Nutrition and What is a Feeding Tube?
While it may sound overly complicated, “enteral nutrition” really just refers to the delivery of liquid food, water, and medication to the digestive system. And the “feeding tube” is the medical device that makes enteral nutrition possible. Think of it like this, enteral nutrition is basically a magic trick that allows kids to take in proper nutrients and stay hydrated. And the feeding tube is the magic wand that makes it come to life! But why would someone need a feeding tube in the first place? As per the “Guide To Tube Feeding For Patients and Families,” which has been kindly published as an online PDF (here) by the Michael Garron Hospital, there are many medically necessary reasons for using a feeding tube. These include when patients:
And what really makes a feeding tube impressive is its versatility. There is not just one type of feeding tube. Instead, there are many kinds of tubes that all have a similar function, but work a little differently. Feeding tubes are classified in two important ways. The first being how the tube is inserted, as they can be placed through the nose or through the abdomen (surgically). And the second being where the tube ends in the digestive system, either in the stomach or intestine. With that being said, there are two main categories of feeding tubes: nasal feeding tubes and surgically placed feeding tubes. First, let’s talk about nasal feeding tubes. These are long, skinny tubes that are really flexible. A doctor will carefully place a nasal feeding tube by passing it through the nose, then down the throat and through the esophagus, before it reaches its final destination in either the stomach or the intestine. Part of the tube must be kept outside of the body so that it can attach to a syringe used for feeding. Taller kids will have longer nasal tubes, while shorter kids will have shorter nasal tubes. The simple reason for this is because the length of the tube is dependent upon the size of the child. Within this category of nasal feeding tubes, there are:
Sometimes, when a feeding tube is needed long-term or even permanently, or if a child just can’t have a nasal tube, the surgically placed feeding tube becomes the best option possible. These tubes are usually inserted by using a laparoscopic procedure, which is a surgery performed with a tiny camera that lets the doctor see the inside of the body through a video monitor. In order to do this, the doctor must make a very tiny cut on the abdomen (stomach). This small opening becomes known as the “stoma.” It is a surgically made hole that heals with time and shouldn’t be painful afterwards. Surgically placed feeding tubes include:
When a PEG tube is placed, first, a small cut (stoma) is made in the upper abdomen, then, the tube is inserted through that stoma, and finally, the tube gets connected to the stomach. About six to twelve inches of the tube will be visible coming out of the site where the small cut was made and through which the tube was placed. An external bumper is placed outside of the tube to prevent the tube from going further into the stomach or becoming easily dislodged. At the end of the tube that is not in the stomach is a small plug, which prevents stomach acid from exiting the tube. When the plug is opened, it is used for providing medications, as well as food and water. Once the stoma is fully healed, and it is clear that the PEG tube has been functioning properly and delivering nutrients, water, and medications as intended, some children may have the opportunity to switch to a G-button. A gastrostomy button, aka the “G-button,” is a more discrete tube that lays on top of the abdominal wall. It is held in place by a balloon, as seen in the diagram below, which was provided by the University of Iowa Stead Family Children’s Hospital, which also has a lot of great information on cleaning, caretaking, and problem solving with G-buttons. When it is time to administer medicine or food, a longer extension tube is attached to the G-button. Whether you have a PEG tube or a G-button, either way, it is possible to deliver both bolus feedings and continuous feedings. These are two very different enteral nutrition options that you may hear of from your gastroenterologist. Bolus feedings require a bolus connector and a small syringe, and occur over 10-20 minutes. Whereas continuous feedings require a continuous feeding connector, feeding bags, and a special bump; they take place over 8-24 hours. If you are still looking for more information on tube feeding, Tubefed.com by Avanos is yet another excellent resource and comprehensive guide to all things related to feeding tubes and enteral nutrition. With so many options available for enteral nutrition delivery, it is crucial to coordinate with your provider, and ask about what tube is best for you or your child. However, don’t be afraid if you try one or two or three different feeding tubes before you find the option that is right for you and your family! What’s most important is that nutrition is received in any way possible, no matter the style of feeding tube. As always, the information provided by this article is merely for informational purposes. This article is meant to offer additional insight, not make any diagnoses or take the place of the opinions of medical professionals. Always consult your team of health care providers for sound medical advice. |
|
NG Tubes:
The nasogastric tube, better known as the NG tube, is a common type of nasal feeding tube. “Nasogastric” means “nose to stomach,” which refers to exactly how this feeding tube functions! Insertion of an NG tube does not require surgery, but rather, the clinician, such as a doctor or nurse practitioner, places the tube into your nasal cavity, so that it can pass through your throat, then into your esophagus, and finally end in your stomach. This way you can still receive proper nutrition. According to the Cleveland Clinic, NG tubes are “[...] designed to be used for up to six weeks,” so, “[...] if you end up needing enteral nutrition for longer than that, your healthcare provider will recommend switching to another kind of feeding tube.” It is suggested that this tube is replaced every 3 days to 4 weeks to maintain good hygiene and avoid infection. If you are discharged from the hospital with an NG tube, your provider will train you on how to take care of your tube, including how to clean it and how to replace it. There are two types of NG tubes: single lumen and double lumen. Single lumen NG tubes are used to deliver liquid food and medications into your stomach via a single, narrow channel. The small diameter of the tube is meant to minimize any discomfort, and allow the tube to be removed and replaced with ease. Two popular models of single lumen NG tubes include the Levin and the Dobhoff. Double lumen NG tubes, on the other hand, are designed to suction air and fluid from the stomach without damaging your stomach lining. As you might have guessed, the double lumen NG tube has two channels, a larger one used for suctioning and a smaller one that relieves pressure by acting as an air vent. The Salem Sump is the most popular model. ND Tubes: The nasoduodenal tube, commonly known as the ND tube, is another example of a nasal feeding tube. An ND tube is similar to an NG tube, since both enter your body via the nasal cavity, but what makes an ND tube unique is that it extends beyond the stomach and goes into the duodenum. The duodenum is the first part of the small intestine. It absorbs nutrients (like proteins, carbs, fats, vitamins, minerals, etc.) and helps to further digest food that comes from the stomach. Furthermore, ND tube must be fitted and placed by a trained clinician. Usually, an x-ray monitor is used to help place this soft feeding tube into the duodenum, which means the patient is sedated or placed under anesthesia for their comfort. Because the ND tube must be strategically positioned in the first part of the small intestine, it is important to note that they should not be replaced at home. If your ND tube becomes dislodged, it is recommended that you return to your provider as soon as possible, so they can replace the tube. NJ Tubes: Another type of nasal feeding tube is the nasojejunal tube, which is better known as the NJ tube. It is comparable to the ND (nasoduodenal tube), except the NJ tube ends in the jejunum. The jejunum is the middle portion of the small intestine, which is sandwiched between the first part of the small intestine (the duodenum) and the last part of the small intestine (the ileum). The main function of the jejunum is to continue digesting food that has passed through the stomach. It also absorbs both nutrients and water, which the body stores and uses for energy. “Post-pyloric feeding,” according to the Journal of Pediatric Gastroenterology and Nutrition, is a way to deliver nutrients directly to the duodenum or the jejunum. “Post-pyloric” refers to digestion beyond the pylorus, which is the main valve involved in digestion. NJ tubes are often used as a route to deliver nutrients to children as a means of post-pyloric feeding. For some patients, post-pyloric feeding is a better alternative to gastric-tube feeding, sometimes due to patient safety and other times just due to its effectiveness. Because NJ tubes end in the jejunum, they must be placed by a trained medical professional. It is rather common for x-ray imaging or endoscopy to be used in order for doctors or nurses to better visualize this part of the body, and ensure that the tube is correctly positioned in the middle part of the small intestine. |
|
G Tubes:
The G tube, which is short for gastronomy tube, refers to the surgically placed feeding tube that is inserted via a small incision (cut) in the skin. G tubes feed directly into the stomach. A balloon filled with sterile water stays inside the stomach and is used to hold the G tube in place, so it doesn’t get dislodged. And a bumper (small disc) stays on the outside of the belly so that the G tube is held in place correctly. A port can be easily opened and and closed in the G tube, so that food, water, and medicine can be easily delivered. Similar to a PEG (Percutaneous Endoscopic Gastronomy) tube, the G tube is inserted via the abdomen (as opposed to the nasal cavity), and is usually used for administering long-term feeding. However, G tubes are not usually placed until after a PEG has been placed and the stoma heals correctly. It is also important to note that G tubes can have either a normal length tube or a low-profile tube, which stays closer to the skin, and is easy to disguise beneath clothing. While they are not always an option for every patient, low-profile tubes are usually preferred because they can be more easily hidden, and they allow for better mobility. Low-profile tubes are less likely to get pulled out or caught on something and misplaced. While G tubes require a surgical procedure in order to be placed, once the clinician approves (and after the stoma has healed), it is safe for a G tube to be replaced at home. GJ Tubes: The (GJ) gastrojejunal tube is another type of surgically placed feeding tube. This type of tube enters through the stomach but extends into the middle part of the small intestine. It requires a small surgery to be initially placed via the abdomen, just like the G and J tubes, however, the GJ tube has some pretty cool features. Essentially, it combines the best parts of G and J tubes into one multi-faceted feeding tube. The GJ tube also has three openings, known as ports. The first port, the gastric port, opens up to the stomach, where it can provide fluids and liquid medications. This port also allows for the removal of any air or fluid that is trapped in the stomach. The second port, the jejunal port, is used for nutritional feedings, so it is connected to the jejunum. And lastly, the third port, the balloon port, helps to fill the balloon with sterile water, so that the tube is held in place. The GJ combines the functions of both G and J tubes to allow for more flexibility for longer term care. However, GJ tubes cannot be replaced at home. J Tubes: The J tube, or the jejunostomy tube, is another type of surgically placed feeding tube that enters through a small cut (incision) in the abdomen, but the J tube specifically reaches the middle part of the small intestine. This is known as the jejunum. J tubes are rather common for long-term care, and provide patients with the opportunity to have a standard-length tube, or a low-profile button tube (though the latter is usually preferred). J tubes are most often placed when people experience slower than normal digestion, and thus, the J tube should prevent reflux. Acid reflux occurs when stomach acid continuously flows back into the tube that connects your mouth and your esophagus. Because J tubes extend beyond the stomach, it is important to note that J tubes cannot be replaced at home, and must be changed in a hospital or other place of medical care. In order to function properly, it is critical that they are positioned in the stomach accordingly. |
Service Animals
Service animals can be a great support system for children with a rare disease or chronic illness
-
About the Author(s)
-
All About Service Dogs
<
>
About the Author(s)
|
My name is Kaylee and I am a senior in high school. I have Complex Regional Pain Syndrome, Occult Tethered Cord Syndrome, Chiari Malformation, and many more diagnoses. My service dog, Chance, is a 2-year-old Bernedoodle. He is a multipurpose service dog who does seizure alert, mobility, and behavior disruption. I have had Chance for just around 9 months! Chance was trained out in Ohio at a training facility. He started training when he was eight weeks old and when he was around a year old he moved to advanced training. Although he is fully trained we still train multiple times a week and are always working on new skills. Thank you for taking time out of your day to read “All about Service Dogs”!
|
|
All about Service Dogs
By: Kaylee Mescal and Chance the Service Dog What is a service dog? A service dog is a dog specifically trained to perform tasks to help an individual with a disability. There are multiple types of service dogs including but not limited to mobility, seizure alert, diabetic alert, and cardiac alert. They are working dogs, not pets, and should be treated with respect as they have a very important job. Where are service dogs allowed to go and what can businesses ask? Service dogs are allowed to go anywhere that their handler(owner) goes. Things like allergies or a fear of dogs are not valid reasons to refuse a service dog. Businesses are legally allowed to ask two questions. First is if the dog is a service animal and second what tasks the service dog is trained to do. “Certifications” or “IDs” for service dogs are NOT real things. What are some tasks a service dog can do? All service dogs are trained for specific things and can also be trained in different ways. While some seizure-alert dogs will bark at you to alert you to oncoming seizures, others will just stare at you and not let up or be interested in anything else. Some general commands that almost all service dogs do are heel, under, down, sit, stay, come, and many more. A heel is when the service dog walks very closely to your side. When their handler stops walking or wheeling they will as well and can anticipate it beforehand. Most service dogs are trained to heel on the left but each service dog is different. Personally my service dog, Chance, heels on the right since my left side is weak and not very predictable. Another more specific command is “button” where the service dog will either use their face or paw to hit the “push button” that opens the door. Another specific command, one that I personally use, is bark. If I start to choke my service dog will start barking and keep barking until my mom comes. What should you not do? You should not pet, bark at, talk to, make noises, take pictures, or do anything along these lines. Additionally do not stare. The service dog and handler are just trying to get on with their normal life, just like anybody else. Their day-to-day life might look a little different to yours but that doesn't mean they want to be stared at. If you are distracting the service dog they can miss an alert which then causes danger to their handler. If you do want to talk or ask a question, talk directly to the handler, not the service dog. Some handlers may be open to answering general questions, while others may not and that is completely okay because it is their personal business. You can help them by treating them like any other person. What to do if a service dog comes up to you without their handler? If a service dog comes up to you without their handler you should follow the dog. They are trying to get help for their handler. As you follow you should still not touch them as it could be a distraction and their handler needs help. |
Additional Things To Add
- Child Life Services
- Teen coping ideas/resources
- Collaborative playlist
- Mobility aids
- Medical devices/equipment
- Surgery
- Going to the hospital packing suggestions
- Symptom relief
- Accessibility
- College tips from rare college students
- Physical/Occupational Therapy
- Mental Health
- Advocating for yourself as. rare patient
- Parent (Rarent) Resources
- Communication devices
- 504s, IEPs - making school easier for your rare child
- Rare/Chronic Illness Glossary
- Policy in your area/nationally(?)